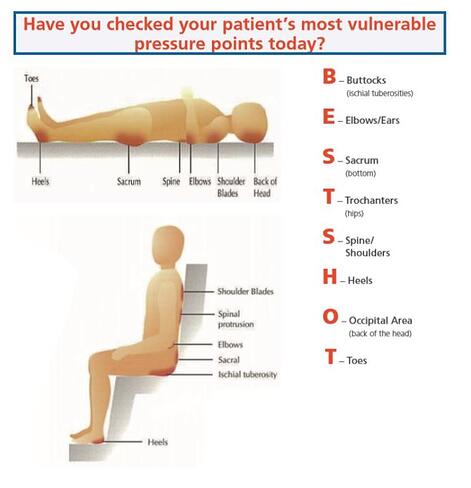
A key study found that when sitting naturally for 1-2 hours, only a small amount could lead to the development of a pressure injury, as body weight in this position is redistributed over a smaller area, resulting in high pressure in the buttocks.
A recent literature review noted the mean prevalence rates of 8.9% in Iceland, 17% in Norway, 16% in Ireland, 15% in Denmark and 25% in Sweden. The USA experiences more than 2.5 million pressure injury cases per year, potentially causing over 60,000 deaths. The UK is no less effected by 70,000 cases per year, resulting in 27,000 deaths.
RISK FACTORS

IMPACT ON THE PATIENT
FINANCIAL COSTS
It is widely acknowledged that many pressure injuries are preventable yet they remain a global problem. There are huge international costs associated with their management and treatment and costs in the UK reach an estimated £1.4 billion – £2.2 billion annually.
The cost to health system in the USA is at least $9-$11 billion dollars and there the USA centers for Medicare and Medicaid do not pay hospitals for the management of pressure injuries as they are considered a medical error.
HUMAN COSTS
The real cost is difficult to define because costs go beyond what we see in the hospital or health facility. There is the dual economic costs to the nation of supporting the individual’s healing and the loss of the individual’s productivity or their family member caring for them. Pressure injuries negatively impacts on quality of life with all the activities of daily living being adversely affected. Worryingly pain is the most common complaints with individuals compounded by the interventions offered to combat risk of further developing pressure injuries.
SOLUTIONS
The NICE guidelines, June 2015, are to be reviewed in August 2018, and are recommend that a patient is repositioned every 6 hours for adults and every 4 hours for high risk adults. However, the frequency or repositioning should be appropriate for the individual person, their wishes and need. For children and young patients at risk, repositioning is recommended at least every 4 hours and more frequently for those at high risk.
The National Pressure Ulcer Advisory Pannel (NPUAP) is the nation’s leading scientific expert on pressure injury prevention and treatment. Their goal is to ensure improved patient health and to advance public policy, education and research.
Regular positioning is not possible for some individuals because of their medical condition and an alternative prevention strategy such as providing a high-specification seating or additional pressure relieving devices may need to be considered.
SEATING MATTERS PRODUCTS
Choosing the right seating and surface influences pressure injury. The chair should be the correct width so the person fits comfortably into the chair. Instability while seated can lead to sliding.
Seating Matters have further demonstrated through the use of their chairs, in clinical field research, carried out in St Camillus’ Hospital, Limerick, Ireland. The field study demonstrated:
- 46% increase of functional tasks.
- 31% reduction in time spent in bed.
- 75% decrease in pressure injury incidence.
- 75% decrease in pain/ discomfort.
- 100% decrease in sliding/ falls.
- 46% decrease in postural correction.
References:
1. National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers. Quick Reference Guide (ed) Haesler E; 2014 Cambridge Media, Perth Australia.
3. Daly O, Casey J, Martin S, Tierney M, and Mc Vey O, 2013. The effectiveness of specialist seating provision for nursing home residents. University of Ulster: Northern Ireland.
4. National Institute for Health and Care Excellence 2015 Pressure Ulcers nice.org.uk/guidance/qs89.
5. Kosiak M. 1959 Etiology and pathology of ischaemic ulcers. Arch Phys Med Rehabil 40(2):62-9.
6. Cook AM, Miller Polgar J, Cook and Hussey’s assistive technologies: principles and practice, third ed. London: Mosbey 2007.
7. Barbanel JC, Pressure management. Prosthetics Ortho Int 1991:15:225-31
8. Defloor T, Grypdonck MH, Sitting posture and prevention of pressure ulcers. Appl Nurs Res 1999:12(3):136-42.
9. Coggrave, M.J, Rose, L.S.(2003) A specialist seating assessment clinic: Changing pressure relief practice. Spinal Cord; 41: 692-695.
10. Bennett G, Dealey C, Posnett J. The cost of pressure ulcers in the UK. Age Ageing. 2004;33:230-5.doi:10.1093/ageing/afh086 CrossRef, Pubmed.
11. Waters TM, Daniels MJ, Bazzoli GJ, et al. Effect of Medicare’s non-payment for Hospital-Acquired Conditions: lessons for future policy. JAMA Intern Med 2015;175:347-54.doi:10.1001/jamainternmed.2014.5486 Google scholar.
12. www.woundscanada.ca/docman/public/health-care-professional/
13. Graves, N.; Birrell, F. and Whitby, M., Modeling the economic losses from pressure ulcers among hospitalised Australians. Wound Repair & Regeneration, 2005. 13(5): p. 462-467.
** This post was originally published on http://blog.seatingmatters.com/pressure-injuries-and-seating


